OCD and trichotillomania share many similarities, but the two disorders differ in their underlying psychobiology. These differences necessitate the use of differing treatment approaches. In a recent study, two groups of patients with OCD and TTM were compared. In the combined group, OCD symptoms were less common than in the OCD-only group. Interestingly, this finding was consistent across both studies, suggesting that the two disorders fall along different dimensions of the OCD spectrum.
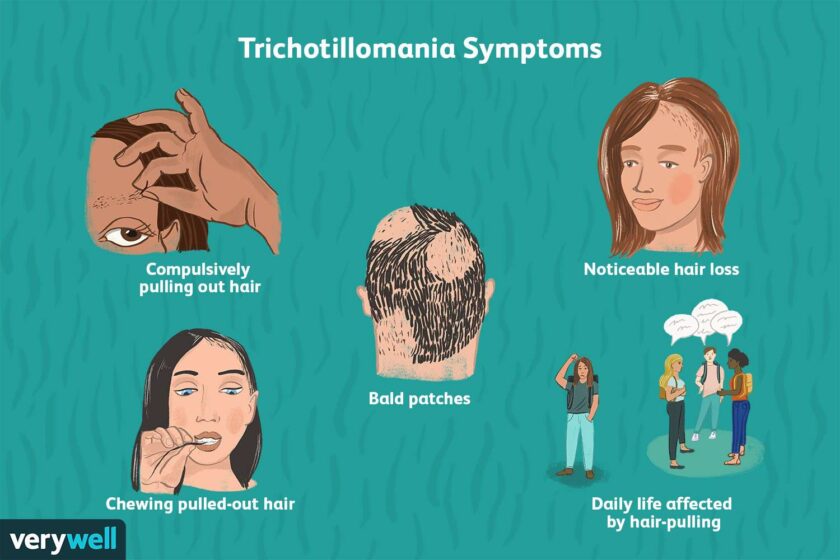
The main symptoms of trichotillomania are compulsions that cause hair pulling. These urges often coincide with strong emotions. In some cases, people with trichotillomania perform their hair-pulling habits as a coping mechanism or to receive pleasurable gratification. But while these behaviors are similar to obsessive-compulsive disorder (OCD), they are not as severe or as pervasive as those of OCD.
A therapist can help those with trichotillomania overcome these urges through habit substitution therapy. In this treatment, people learn to recognize the specific triggers of their hair-pulling urges. They also learn to recognize when their urges subside, when they get stronger, and how to cope with stressful situations and times. A therapist can also provide help to people with nail-biting and perfectionism.
Treatment for trichotillomania usually involves a combination of psychotherapy, medication, and/or other forms of therapy. For some, intensive therapy is necessary to manage the symptoms, while for others, the disorder is best treated in a supportive environment. Although it is often associated with emotional distress, it can be treated successfully by a trained therapist. If treatment fails, it is recommended to consider a course of action that will help patients recover.
Treatment for trichotillomania OCD is not easy. In most cases, therapy involves cognitive therapy and habit reversal. During this therapy, individuals learn to substitute other behaviors for their hair pulling, such as social situations, friendships, and jobs. The therapy can also address distorted beliefs that accompany the condition. It is important to choose the treatment that is right for you, as you may have to try several methods before you find the one that works for you.
Often, people with this condition experience significant distress as a result of their impulsive behaviors. In addition to the physical distress caused by hair pulling, people with Trichotillomania may feel embarrassment or shame. They may avoid being in social situations, and they may even attempt to hide their disorder by wearing wigs or false eyelashes. These symptoms can cause a person to suffer from a significant reduction in self-esteem and even lead them to abuse substances. Trichotillomania affects one to four percent of the population.
Researchers have identified four components to treating trichotillomania. A four-component approach based on the negative reinforcement theory has been successful in reducing the recurrence of hair-pulling. The first component of the therapy involves examining an individual’s pattern of hair-pulling. The second component involves creating a hair-pulling hierarchy based on the intensity of premonitory urges in different scenarios. The fourth component utilizes exposures based on the hierarchy of the individual. Exposures to these scenarios are then used to encourage individuals to hold their hair until the urge goes away.
In addition to behavioral treatments, the study team also compared the symptoms of trichotillomania with those of OCD. The study team used several psychometric tests, including the Yale-Brown Obsessive-Compulsive Disorder Severity Scale, the Massachusetts General Hospital Hair-Pulling Scale, and the Trichotillomania Behaviour Profile.
The brain regions affected by trichotillomania have undergone extensive structural alterations. The brain regions responsible for motor habit generation, suppression, and affective regulation are also disorganized. Ultimately, trichotillomania is an impulse control disorder, and it needs to be addressed. Treatment can help the sufferer improve their quality of life, remission of symptoms, and overall quality of life.
The comorbidity of trichotillomania and OCD is substantial. Patients with TTM and OCD were significantly more likely to be affected by other psychiatric conditions. The prevalence of TTM and OCD in TTM patients was higher than in the OCD group. In addition, comorbidity between OCD and TTM was also higher. A higher incidence of pathological doubting was seen in the TTM group compared to the OCD group.
While trichotillomania is not a serious disorder, it can be embarrassing and affect the sufferer’s self-esteem. In addition to the shame and embarrassment caused by the condition, hair pulling is often used as a coping mechanism. Treatment for this condition can help the sufferer stop the hair pulling. It is not abnormal or dangerous, and treatment can be found to help the sufferer cope.